Here’s what you need to know about Lymphoedema
Being diagnosed with lymphoedema can cause uncertainty, frustration, and a lot of unanswered questions. From understanding the causes to finding effective ways to manage symptoms, it’s natural to feel unsure about what lies ahead.

At Amoena, we have over 50 years of experience in breast care. We’ve pioneered innovations such as silicone breast forms and post-mastectomy lingerie and swimwear, working closely with medical professionals and women around the world to design products that are comfortable, effective, and empowering.
Whether you’re living with lymphoedema yourself or supporting someone you love through it, this guide is intended to provide guidance, reassurance, and practical tips to help you manage both the physical and emotional aspects of this condition.
When I was first diagnosed with lymphoedema, I felt overwhelmed and unsure of what life would look like. Learning that it could be managed — and that I wasn’t alone — made all the difference.— amoena Ambassador
This guide is designed in two parts: the first for those navigating life with lymphoedema, and the second for those supporting a loved one.
Part One: If You’re Living with Lymphoedema
What is lymphoedema?
Lymphoedema is a long-term condition that causes swelling, most often in the arm, hand, or chest area, after lymph nodes have been removed or damaged, commonly during breast cancer surgery or radiation treatment. It occurs when lymph fluid (which normally helps remove waste and protect against infection) can’t flow properly and begins to build up.
With early recognition, regular care, and the right support, lymphoedema can be managed effectively. Over time, many people find they can keep symptoms well under control day to day.
Common lymphoedema symptoms
- Swelling in a limb or other part of the body (e.g., arm, hand, leg, foot) that causes clothes, shoes or jewellery feel tighter
- A feeling of heaviness, tightness or fullness in the affected area
- Aching, tingling, numbness or general discomfort
- Skin changes: the skin may feel tight, look discoloured, thicker or less flexible; possibly pitting (where a pressure leaves an indent)
- Decreased range of motion or stiffness in the joint near the swollen area
- Recurrent skin infections, or skin in the area becoming hard, thickened or developing folds
Stages of lymphoedema
In the early to moderate stages of lymphoedema, symptoms often appear gradually and may come and go. You might notice swelling that worsens during the day and eases overnight, a feeling of heaviness or tightness, or mild pitting when the skin is pressed. Clothing or jewellery may start to feel snug, and movement in the affected area can become slightly restricted.
Over time, if lymphoedema progresses without consistent management, the swelling can become permanent and the skin may begin to harden or change texture. In advanced stages, the skin can appear dry, thickened, or discoloured, sometimes developing small growths or fluid leakage. These changes can make movement more difficult and increase the risk of infection, which is why early recognition is so important.
At first, the swelling came and went, so I didn’t think much of it. Looking back, those early signs were my body asking for care.— amoena Ambassador
Parts of the body most often affected by lymphoedema
Lymphoedema can develop in almost any part of the body, but it most commonly affects the arms and legs, where swelling is usually most visible. This is often linked to lymph node removal or radiation therapy following breast cancer treatment.
In some cases, it can also appear in the head, neck, chest, abdomen, or genital area if the lymphatic system is unable to drain fluid properly. Wherever it occurs, symptoms like swelling, heaviness, or tightness, are caused by the same underlying issue: a blockage or disruption in the body’s natural lymph flow.
Ways lymphoedema is managed and treated
Lymphoedema is a chronic condition but there are effective ways to manage it and reduce discomfort.
While Amoena is not a medical specialist, we’ve worked alongside healthcare professionals and women living with lymphoedema for decades, so we understand the importance of proper care and guidance. Every case is unique, so it’s always essential to speak with your doctor or lymphoedema therapist about the best treatment plan for you.
The recommended medical approach for lymphoedema is known as decongestive lymphatic therapy (DLT). Although it’s not a cure, DLT helps to manage symptoms, reduce swelling, and prevent the condition from progressing. Treatment is usually tailored to your individual needs.
DLT includes:
- Compression therapy: Compression sleeves, bandages, or garments support the affected area and help move fluid away from swollen tissues.
- Skin care: Keeping your skin healthy and moisturised helps prevent infections, such as cellulitis, which can make swelling worse.
- Exercise and movement: Light, regular activity encourages lymph fluid to flow more freely. Simple stretching, walking, swimming, or cycling can all support healthy circulation, always under your doctor’s advice.
- Manual lymphatic drainage (MLD): This is a specialised massage technique performed by trained therapists to stimulate lymph flow and reduce swelling. Over time, you may be taught self-massage techniques to continue at home.
In some cases, surgical options such as liposuction or procedures to redirect lymph flow may be considered at specialist centres. These are typically reserved for more advanced or persistent cases and should be discussed with your medical team.
Read more about lymphoedema treatmentLiving with lymphoedema
A lymphoedema diagnosis can feel daunting at first, and swelling and visible changes can affect how you feel about your body.
Practical tips:
- Build a simple self-care routine you can maintain daily.
- Wear breathable fabrics and avoid tight jewellery or sleeves.
- Talk to others living with lymphoedema through local or online support groups. The Lymphoedema Support Network is a good place to start.
Emotional wellbeing is as important as physical care. Journaling, counselling, or simply talking to a trusted friend can help you process frustration or body image concerns. Over time, most people find a rhythm that feels normal again.
Read more about coping with lymphoedema
Creating a simple daily routine changed everything for me. Small, consistent steps made lymphoedema feel manageable instead of overwhelming.— amoena Ambassador
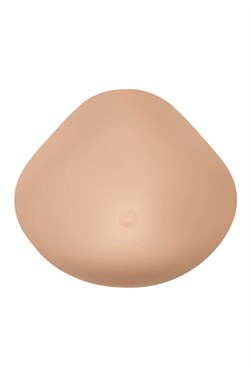
Supportive products from Amoena
Amoena’s products are thoughtfully designed for women recovering from breast surgery and managing lymphoedema. Amoena’s CuraLymph range is a specialised collection of compression garments, comfort wear, and accessories designed to support women managing lymphoedema after breast surgery by promoting healthy lymph flow, easing swelling, and providing everyday comfort and confidence.
Read more about lymphoedema brasPart two: supporting someone with lymphoedema
When someone you care about is diagnosed with a chronic illness, it can be hard to know how to help. In the case of lymphoedema, they may feel frustrated, self-conscious, or anxious about long-term management, but your patience and encouragement can make a world of difference.
How to support someone with lymphoedema
- Be patient: Lymphoedema management takes time and daily care
- Be practical: Help with everyday tasks, from carrying bags to reminding them to rest.
- Be reassuring: Body changes can impact confidence. Gently remind them that they’ve got this!
- Be informed: Learn about lymphoedema after breast cancer so you can understand what they’re going through.
Connecting with others who understood lymphoedema made me feel less isolated. Shared experiences can be incredibly powerful.— amoena Ambassador
Common FAQs about lymphoedema
What causes lymphoedema after breast cancer?
It’s usually caused by damage or removal of lymph nodes during surgery or radiation therapy, which affects fluid drainage in the arm or chest area.
Can lymphoedema be cured?
It can’t be completely cured but it can be managed effectively through compression, exercise, skin care and regular monitoring.
What are early signs of lymphoedema?
Early signs can include a feeling of heaviness, tightness, or swelling in the arm or chest, especially after exercise or heat exposure.
Can I exercise with lymphoedema?
Yes, movement supports lymph flow. Avoid heavy lifting or repetitive strain and follow your physiotherapist’s guidance.
Why is physical activity helpful for lymphoedema?
Exercise supports lymph flow by encouraging your muscles to contract, which helps move fluid away from swollen areas. It also keeps joints flexible, supports a healthy weight, and can ease feelings of tension.
Are there any exercises I should avoid with lymphoedema?
You can use your affected limb for most everyday activities, but it’s best to avoid exercises that cause strain, pain, or discomfort. If swelling increases, your skin becomes red or hot, or you feel unwell, stop and rest. Avoid exercising if you have a skin infection (such as cellulitis) and speak to your healthcare professional.
Should I wear my compression garment when I exercise?In most cases, yes. Compression sleeves or garments help maintain healthy lymph flow during physical activity. If you find them uncomfortable, talk to your lymphoedema specialist, who can suggest adjustments or alternative options.
How can I position my arm or leg to help reduce swelling?
When resting, try to raise the affected limb slightly above heart level to encourage drainage. For arm swelling, rest your arm on a cushion or chair arm to keep it supported. For leg swelling, elevate your feet on a stool or pillows when sitting or lying down, and avoid crossing your legs or standing still for long periods. Small posture adjustments throughout the day can make a big difference in comfort and control.