Coping with Lymphedema
What you need to know now—and new strategies in the works
 Do you have lymphedema or are you concerned you might develop it?
Do you have lymphedema or are you concerned you might develop it?
Lymphedema can develop immediately following breast cancer treatment, but sometimes symptoms don’t appear until months or even years afterwards.
We find out how surgeons, specialists and support communities help women manage the condition.
If you've had breast cancer surgery or radiation, you may have developed lymphedema as a result.
If so, you're not alone: lymphedema affects one in five women who have breast cancer treatment. Yet despite this sizeable statistic, it seems information about the condition is not consistently provided by healthcare professionals. This could be because the focus for a woman's medical team is to cure her breast cancer — a life-threatening disease — and some see lymphedema as a relatively mild potential side effect.
Whatever the reason, many women, unaware of the risks and causes, are understandably frightened and confused when they first experience the symptoms.
Stay in the flow
The lymphatic system is one of the body's natural
If the system is damaged, the lymphatic channels can get blocked, which results in fluid pooling in the limbs and causing swelling. This uncomfortable condition is known as secondary lymphedema (as opposed to primary lymphedema, which is caused by a genetic disorder).
Secondary lymphedema is often a symptom of breast cancer treatment because of damage caused by either surgery or radiation. The first signs include a feeling of heaviness, usually in the arm, tightness in the skin and swelling in the affected area.
"Results are much better if treatment of the condition is started in its early stages," he says. "Yet often a woman will go to her medical team in some discomfort and be told that they can't help her. It's only then that she may start to look around for information and help from elsewhere."
Along with around 200 other registered lymphatic therapists in the U.K., Michael uses a special type of massage called Manual Lymphatic Drainage, or MLD. This treatment, sometimes combined with multi-layer bandaging, together with simple daily exercises, can dramatically reduce lymphedema symptoms and make the condition manageable. Developed back in the 1930s, there are several different types of MLD techniques including Vodder, Leduc, Földi and Casley-Smith, and it is important to seek out a trained, qualified therapist.
Self help
If you do have lymphedema, whether you’re treated at your local hospital or seek the services of an MLD specialist, there are some self-help measures that can improve things for you. Check our list of resources below.
You could also try SLD – simplified lymphatic drainage, a form of MLD that can be taught to patients to help them keep their condition under control once the volume has been reduced with MLD and multilayer bandaging. Taking care to wear your compression garment, if you have one, and ensuring that you protect the affected limb, will also help.
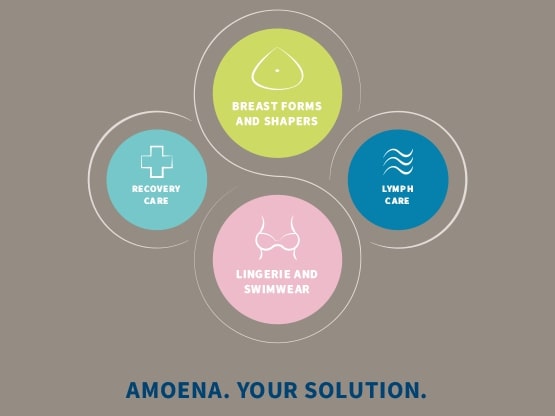
>> Lymphedema can also take place in the breast or chest; for that, Amoena has developed a unique lymph care concept. Read about our compression garments for lymphedema here.
Whether or not you have lymphedema, Michael advises eating a balanced diet and drinking plenty of water to flush out and eliminate toxins. Regular exercise also helps stimulate lymph flow. "Bouncing on a mini-trampoline a few times a week is great," he says. "When you bounce on a trampoline you are flexing your muscles, raising your pulse, and it's a softer landing than jumping up and down on the floor."
Could further surgery help?
Pioneering specialists the world over are working hard to offer lymphedema sufferers surgical solutions, including lymph node transfer, where healthy lymph nodes are transferred from a ‘donor site’ on the body to the damaged site, to try and restore healthy lymph flow. Another procedure involves ‘supermicrosurgery,’ where vessels of less than a hair’s breadth are joined under an operating microscope.
These processes are not widely
Resources:
Professional Association of Manual Lymphatic Drainage practitioners, www.mld.org.U.K.
Michael Villemin, MLD practitioner, http://www.santeaunaturel.co.uk/
Lymphedema Support Network, www.lymphedema.org
Oxford Lymphedema Practice, www.olp.surgery
HealthUnlocked, www.healthunlocked.com