Girl Talk: Get the Breast Cancer Info You Need
Jo Franks, a breast surgeon, gives women the space they need to talk about breast cancer issues and decisions.
When diagnosed with breast cancer, it’s crucial that women are given the information they need to select the treatment option that’s right for them. Too often, says leading breast surgeon Joanna Franks, they feel pressured, afraid and ill-informed.
 Jo Franks is a breast and oncoplastic surgeon and lead consultant at UCLH (University College London Hospital).
Jo Franks is a breast and oncoplastic surgeon and lead consultant at UCLH (University College London Hospital).
Like many people who become doctors, Jo knew from the age of about two that she wanted to go into medicine, and when the time came to choose her vocation, she chose to become a surgeon: “We treat disease, whereas medics just control it,” she explains. “I decided to specialise in breast surgery because I felt it was a field where I could really make a difference.”
Asked what she particularly loves about her work, Jo explains it’s the chance to connect with patients. “I know I am taking them on a very difficult journey but I want to leave them feeling positive at the other end.” She believes it’s vital for women to feel they have a connection with their medical team: “Everyone is entitled to a second opinion on the NHS—not many people know that. So do be sure you feel comfortable with your surgeon and the entire team—after all, you’re going to be entering into a therapeutic alliance with them.”
Lumpectomy v's . Mastectomy? Take Time to Make the Decision
When a woman is diagnosed with breast cancer, it is a huge shock, and
“Being told you have breast cancer doesn’t mean you must have an emergency operation,” she explains. “For most
Long-term Breast Surgery Outcomes
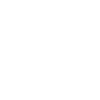
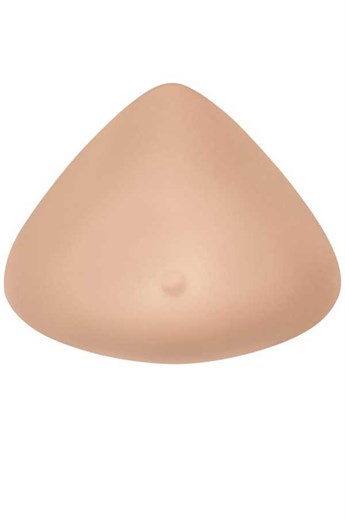
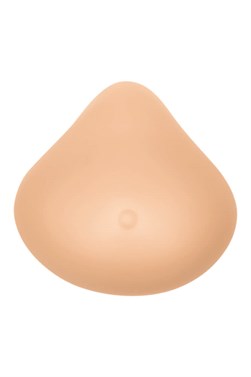
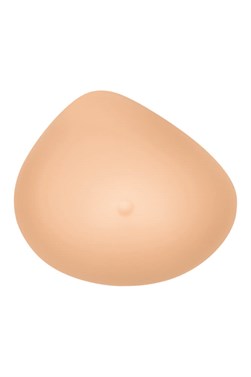
 How are medical teams helping women become better informed? “At my practice, if you are given a breast cancer diagnosis and treatment options you are never asked to make a decision at that point,” says Jo. “You have an appointment with a clinical nurse specialist, look at photographs, feel implants and silicone breast forms, ask questions about the procedures, and then— when you are ready— you give your consent at a subsequent meeting with me.”
How are medical teams helping women become better informed? “At my practice, if you are given a breast cancer diagnosis and treatment options you are never asked to make a decision at that point,” says Jo. “You have an appointment with a clinical nurse specialist, look at photographs, feel implants and silicone breast forms, ask questions about the procedures, and then— when you are ready— you give your consent at a subsequent meeting with me.”
Girl Talk: A Pre-surgery Support Group for Breast Cancer
“At our regional plastics
“I’d love to see more groups like this taking place. We women are very good at supporting each other —we just need the right environment to do it in.” Local breast cancer support groups and mastectomy boutiques might consider partnering with breast care doctors, who could refer patients to these “pre-surgery” information sessions. It’s just this kind of ‘girl talk’ that really helps patients feel educated, informed, and less alone.
Facing Breast Cancer Prepared: It Helps to Know what’s Available
“When I do a mastectomy without reconstruction for whatever reason, I tell women there is specially designed mastectomy lingerie, pocketed swimwear and breast prostheses that mean they can do everything they did before, and no-one will ever know. Partial breast shapers and the right lingerie can also help with asymmetry in the case of reconstruction.
“The thing is, if you haven’t had to face this before, you would have no idea what’s out there. Knowledge is power.”